A while later Donna, the nurse practitioner for the NICU, came to our room to discuss Hannah and her situation. We were given the estimate of a 2 week stay in the NICU. Despite being a heavy weight for a 35 weeker (she was 6 lb 5 oz while the average for her gestational age is about 5 1/2 pounds), her lungs were severely underdeveloped. She fell into a category of about only 10% of 35 week babies that have Respiratory Distress Syndrome. This is a lung disorder where surfactant, the liquid that coats the inside of the lungs and helps them stay open and move smoothly while breathing, is lacking. Without surfactant the baby has to work harder to breath, and in Hannah's case this was seen in her rapid, shallow breaths, grunting while trying to breath, and severe pulling in her chest muscles where she was having to pull hard for a good breath and the lungs were sticking.
We were told she had been put on a CPAP to help push additional air into her lungs and was delivering about 45% oxygen to her. She was being watched closely and if her breathing became any more labored they would intubate her (tube down her throat into her lungs to help inflate them) and surfactant would be added through the intubation. Thankfully it never got to that, and babies generally produce their own surfactant about 2-3 days after birth.
In addition to the CPAP she had an OG tube (orgastric tube) [the orange tube in her mouth being held down with tape] that delivered food into her belly and also helped suck out some air bubbles and gunk that were in her stomach. She had an IV to deliver iv fluids that kept her fed and hydrated for first bit of life. I don't think they introduced colostrum or formula into her OG tube until she was almost 48 hours old. The IV started in her foot but preemie veins are very small and weak and don't last very long, so she went through quite a few iv locations. She also had 2 lines going into her umbilical stump, one in a vein and one in an artery. These made blood draws easier (they were testing her blood gas levels every few hours) among other uses. The UVC (line in the umbilical vein) began inching into her liver so it was pulled after about 24 hours. She kept the UAC (umbilical artery catheter) for a little over 2 days. We were advised and consented to the insertion of a PIC line if need be. This would be a central line going into a main vein in her arm that would be longer lasting than the regular IVs that don't last very long. Again, like with intubation, we were lucky and thankful the PIC line was never needed. She also wore leads that continuously monitored her heart rate, breathing rate and oxygen saturation. She was hooked up to quite a few things. She also went through 2 days of photo therapy for high bilirubin levels, but this is extremely common in preemies.
Because of the magnesium I was on and being unable to walk, I wasn't able to see her until about 30 hours after her birth. And when I did see her, we couldn't hold her and were barely allowed to touch her. They wanted to keep her as unstimulated as possible to give her a chance to rest, sleep and recover.
Seeing her was a shock to my system. She was on her back and her breathing issues were more pronounced since we were able to see the forceful breaths she was taking and hard rise and fall of her chest. Even though I had heard what was going on, seeing my baby hooked up to so many monitors, tubes and lines and the struggle she had to take simple breaths of air was just heartbreaking. I cried. I apologized that I wasn't able to stay pregnant longer. I hugged Andrew and cried again. He had been visiting her throughout the day so he had see the machines and strained breathing already. I wasn't mentally or emotionally prepared for it. I trusted the NICU staff and believed that she would improve, but was fearful in that the first 72 hours are the hardest, and most dangerous for preemies.
On Friday, 9/12, they started giving her my breast milk through the OG tube. They gave her 10 cc of whatever I could provide and supplemented with a preemie formula for the rest, every 3 hours. She immediately seemed more relaxed and happier. The next day it was 20 cc. Then Sat night it was 30 cc. Sunday it was up to 40. I couldn't keep up! She was handling the feedings so well they increased her to what a full term baby would be eating at her age.
I finally got to hold her Saturday evening. We weren't expecting to be able to hold her for a while, but they removed the UAC Saturday morning, and transitioned her from the CPAP to a nasal cannula that evening. With these changes they felt she was stable and strong enough to be held. Andrew was taking a milk delivery down to the NICU for a quick drop off when the nurse asked if he wanted to hold her. Knowing I hadn't held her yet (and he had) he told the nurse we would love to, but he needed to get Mommy first! I was so surprised and excited it took everything I had to not run down the hall to her. And with a 4 inch incision and a bunch of stitches, that would have been a bad idea. I collected my emotions and we headed down.
I was discharged on Sunday, Sept. 14. Leaving the hospital without a baby was one of the hardest and most emotional things I've ever done. I cried, multiple times. It was great to be home, but a major piece of me was missing. We hung out at the hospital for the day and got as many cuddles as we could before leaving.
The entire NICU stay we were warned that it was all on her time table. She could do great breathing, but then get to the eating part and take weeks to learn it. One of the hardest things for babies to do, preemies in particular, is suck, swallow and breath at the same time. For a baby with lung issues, this can be a real hurdle. Not for our Hanny. This girl had plans of her own. She sabotaged an iv one day, so they decided to remove it and monitor her. She kept her glucose levels up for 3 feeds so they decided she no longer needed the iv fluids. They introduced a bottle a day or so later to see how she did. They moved her OG tube to her nose (making it a NG tube) to faciliate bottle feedings. A day later she pulled out the NG tube when a nurse had her back turned. Again the practioner decided to go with it and see how she did under close supervision. Hannah took every bottle feeding like a champ, showing she didn't need the NG tube anymore.
Wednesday, 9/24 when she was 1 week old they decided to let me attempt breast feeding. Getting milk from the breast requires a lot more work than from a bottle, so we didn't expect a whole lot. The hospital Lactation Consultant (LC) came to help us and worked with Hannah and me to have a successful first feeding. I came back that night to try again and she had no interest, but that was ok. We knew she wouldn't do perfectly every time. Thursday morning I returned and tried again with minimal success. But she had been doing so well they offered us the option to 'room in' with Hannah that night.
Rooming in meant we stayed at the hospital in a room next to the NICU, with Hannah in our room as a trial run. She still had her heart rate and breathing monitors (3 small leads attached to her chest that ran to a small monitor), but we got to experience having a baby around! She also got to meet her grandparents from Florida, Andrew's dad and step-mom.
Mommy's 1st diaper change
We got very little sleep that night, as expected. Partially because we had a baby with us, and partially because her monitors were acting up and going off all night for no reason. I thought Andrew might throw the display box out of the window! Despite a rough start with me getting the chills, running a fever and general flu like symptoms (yay engorgement/mastitis!) things calmed down and we made it. We took Hannah back to the NICU nursery early the next morning so I could go to the doctor and we could spend some time with Howard and Tammy.
Andrew had to work a double the next night so I returned alone for night 2 of rooming in and we had a girls slumber party. We both got more sleep that night. We also got the exciting news that she would be released Saturday afternoon! After a visit from Howard and Tammy that evening we tucked in, got some rest and geared up for an exciting Saturday! The NICU was really busy with an influx of babies so they didn't get her discharge paperwork ready until about 2:00 pm. We waited around to see if Andrew would be allowed to leave work for a short while to be a part of baby going home. Sadly CCF was understaffed and he didn't get to make it, so around 4:00 pm Hannah and I loaded up, and headed home.
After 10 long days in the NICU, our girl was being released. I was so excited and nervous all at once. Since Andrew had to work it was just us. When I got in the car a song by Drake was playing and the chorus goes something like "just hold on,we're going home. Going home." It was so fitting.
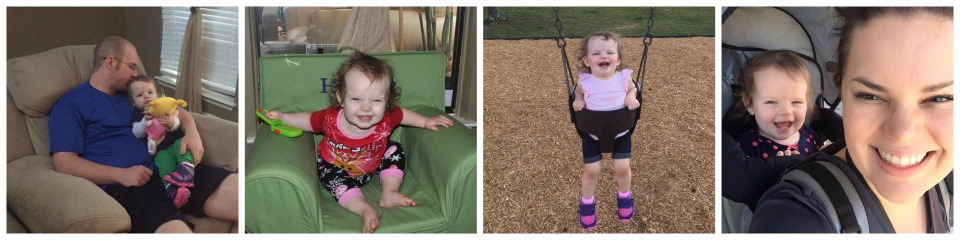
So there ends our NICU journey. 10 long days. Hannah dominated every obstable she encountered and did it faster than most of us expected. The nurses and doctors who took care of her when we couldn't changed our lives forever, and we are so grateful to them. She came home Saturday evening, just in time for my 29th birthday that following Monday!